Hypervolemia
What is Hypervolemia/ Fluid overload?
When the blood vessels in our body carry abnormally high volume of blood, the condition is called hypervolemia (1). In fact, the fluid portion of the blood is higher in this state.
Further in this article, we would be looking at what maintains the fluid balance, how hypervolemia occurs, their causes, clinical features and treatment.
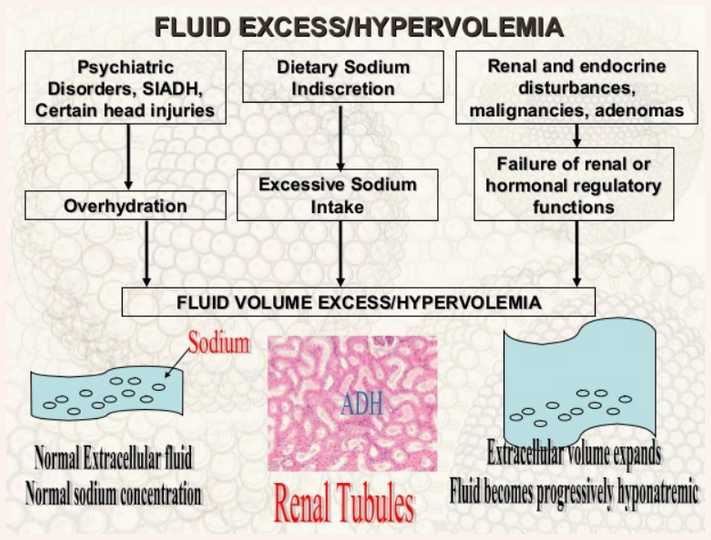
Image 1: Hypervolemia – a general outlook.
Difference between Hypervolemia and Hypovolemia
Hypervolemia is increased volume of blood in the blood vessels whereas hypovolemia is decreased blood volume. See more info on : hypovolemia
Pathophysiology of Hypervolemia
Total body water (TBW) is about 70-75% of the lean body weight in infants to 60% in adults (2). TBW includes intracellular fluid (ICF, fluid inside the cells) and extracellular fluid (ECF, fluid outside the cells). Intracellular fluid makes up around 66% of the TBW (2), whereas extracellular fluid reaches around 33% (2).
Further, ECF is made up of two components, namely, interstitial fluid and the plasma. Interstitial fluid that makes up around 75% of the ECF, occupies the space between the cells. Plasma is the fluid component of blood that constitutes to 25% of the ECF (2, 3).
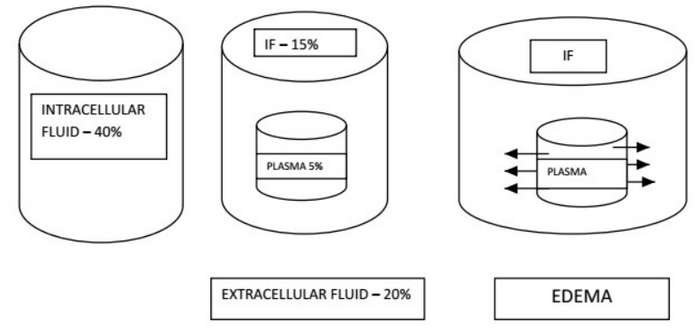
Image 2: An image depicting the distribution of fluid in various compartments of the body.
Plasma which is around 8% of the TBW or around 5% of the lean body weight is increased in case of hypervolemia.
The fluid levels in different body compartments are maintained and balanced by the electrolytes which are present in each compartment. The composition of electrolytes inside and outside the cells is different.
The cell membrane that divides these two compartments is in fact permeable to water but not to electrolytes (2). Where ever the electrolytes are higher, the osmolality is increased, thus resulting in higher levels of fluid. In simple terms, when there is more solute, water is pulled towards that side of the membrane (4).
The main solutes inside the cell are potassium and organic phosphates, while outside the cell they are sodium, chloride and bicarbonate (2). Any imbalances between these solute levels will also shift the water levels within the system.
Sodium levels in the body are regulated by the nervous system (sympathetic nervous system) and hormonal system through the kidneys. This is done by modulating the excretion or retention of sodium (2).
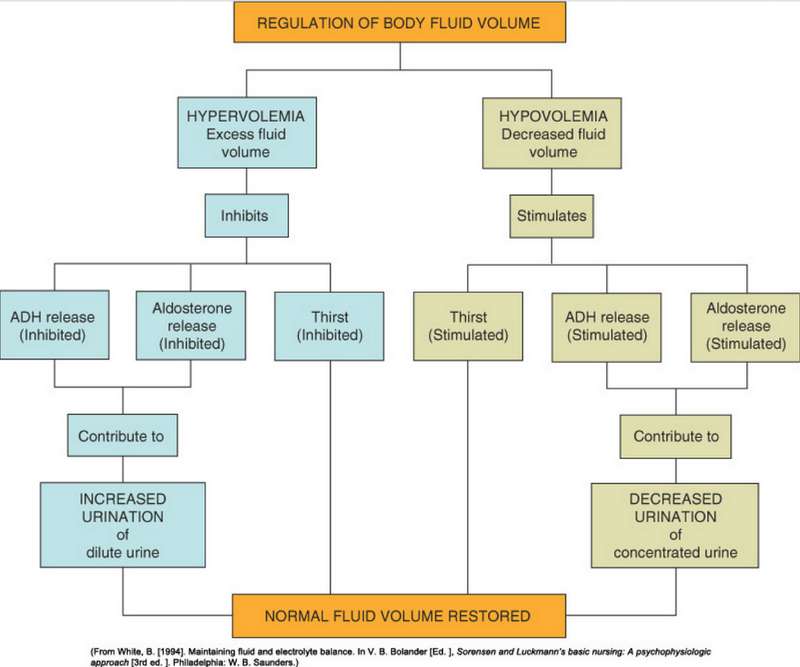
Image 3: A flow chart showing how the body regulates the fluid volume within.
Imbalance in sodium or water levels in extracellular fluid, usually results in one of the four disorders, namely hyponatremia, hypernatremia, hypovolemia or hypervolemia (2).
Hyponatremia indicates a decrease in sodium levels in extracellular fluid, whereas, Hypernatremia is an increase in extracellular fluid sodium. When blood has more water component the sodium becomes diluted, resulting in hyponatremia (2). When blood has too little water, sodium concentration is relatively increased (2).
It is important to understand the reverse too. If blood is having less sodium levels, this will cause the body to lose water resulting in hypovolemia (2). When the sodium levels are higher in blood, this will attract and retain more water, leading to hypervolemia and oedema (2).
The normal level of sodium in the blood is around 135-145 mEq/L (5). When the sodium level in blood goes above 145 mEq/L the condition is called hypernatremia. This most commonly results from fluid loss which is not replaced due to abnormality in the thirst mechanism or due to lack of water (2).
When water is less in blood, sodium is more concentrated. This causes water to be pulled out from inside the cells or more water to be consumed to help the sodium and water levels to be balanced in blood. Hence, hypervolemia ensues.
The intense thirst which occurs due to hypernatremia (increased sodium in plasma) leads to activation of pituitary gland to release a hormone called anti-diuretic hormone (ADH). This acts on the kidneys to retain more water from the urine (2).
What causes Hypervolemia?
Understanding the pathophysiology given above makes it easier to understand hypervolemia causes.
| Cause | Detail |
| Excess IV fluids (7, 8) | Large volume of IV fluid given over a short period of time. Or when hypotonic solutions are given fast. |
| Blood transfusion (9) | Blood transfusion can result in fluid overload if large volume or rapid transfusion is done. |
| Increased Dietary Sodium intake (10) | Increased sodium intake leads to increased fluid intake. |
| Cause | Detail |
| Congestive heart failure (10) | Ineffective pumping of heart causing blood being held in the veins. When the tissues are getting insufficient blood supply, the internal mechanism causes more fluid to be retained in the blood. Thus leading to more of hypervolemia. |
| Nephrotic syndrome (10) | This results in oedema due to protein loss from the body. As a corrective mechanism body tries to retain more fluid and sodium in blood. |
| Glomerulonephritis (10) | Kidney fails to excrete excess fluid. |
| Liver cirrhosis (10) | Plasma levels are increased. |
| Hyperaldosteronism (10) | Aldosterone hormone causes more sodium to be retained in the body, thus resulting in more water being retained too. |
| Drugs (10) | Corticosteroids, Chemotherapy |
| Surgery (10) | Surgery can result in water being retained more. |
| Hormonal disturbances due to stress (10) | Head injury or post-operative patients, ADH may increase. This can result in water retention. |
| Malnutrition (10) | Low protein intake leading to hypervolemia. |
| Cause | Detail |
| Pre-eclampsia (10) | Hypervolemia |
| Pregnancy (6) | Increased renin and aldosterone activity leading to sodium and water retention (6). |
| Cushing’s syndrome (10) | Hypervolemia |
Tables: Tables listing the causes of Hypervolemia
Hypervolemia Signs and Symptoms
Signs and symptoms of hypervolemia may change from person to person depending upon the organ or area in which the water has moved to (11). They may include
- Edema (1) – In hypervolemia, the hydrostatic pressure (pressure that blood exerts on the blood vessel walls and which helps in moving forward) is increased. This causes fluid to escape into interstitial space (space in between the cells), resulting in edema. Edema occurs mainly in feet, ankles and hands (11). (Also see – What is Anasarca)
- Ascites (1) – When edema occurs in the peritoneal cavity, then it is called as ascites.
- Strong rapid pulse (11, 12) – Since the volume of blood is high in the blood vessels, the pulse is bounding and rapid.
- Hypertension (13) – Increased blood pressure in hypervolemia is due to increased volume.
- Elevated central venous pressure (CVP) (13) and pulmonary artery pressure (PAP) (13) due to circulatory overload.
- Raised preload (volume of blood in the right or left ventricles at the end of a diastole) in the heart leads to distended jugular vein (13).
- During the diastole, there is rapid filling of the ventricles and they become overloaded and distended, resulting in third heart sound (13) or S3 gallop.
- Dyspnoea (13) (Difficulty in breathing due to pulmonary oedema) with rapid breathing may be present.
- Orthopnoea (13)– Difficulty in breathing in lying position due to pulmonary oedema.
- Paroxysmal nocturnal dyspnoea (1) – Difficulty in breathing at night which can be due to orthopnoea.
- On auscultation, crackles (13) may be heard in the lung fields.
- Kidney function changes such as oliguria (13) (markedly reduced urinary output), azotemia (13) (elevated blood urea and creatinine)
- Anxiety, restlessness or confusion may be seen in some (13).
- Increased body weight.
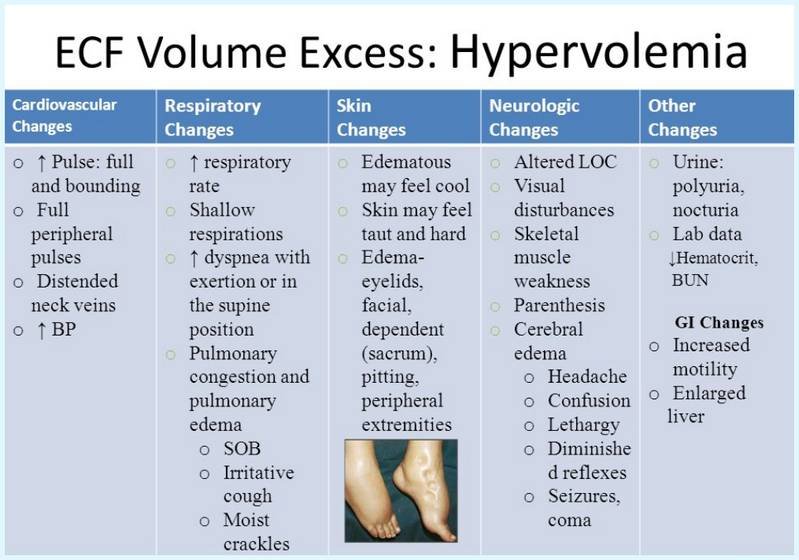
Image 4: Signs and symptoms of Hypervolemia

Image 5: An image showing edema in a patient with fluid overload.
What are the complications of Hypervolemia?
The most common complication seen in case of hypervolemia is congestive heart failure (1). Hyponatremia can also occur in some cases (1). Similarly, in lungs, it may cause pulmonary edema (13).
Hypervolemia Diagnosis
An appropriate history, with adequate examination will give enough cues to diagnose hypervolemia. The patient may complain of breathing difficulties especially at night. They may have swelling on the ankles, feet or hands. Chest examination will demonstrate crackles in the lung field(1, 11, 13).
Investigations can be targeted towards serum electrolytes, blood urea, serum creatinine, urinary output, glomerular filtration rate (GFR) and chest radiography. Electrocardiogram (ECG), echocardiography and abdominal ultrasonography may also be required.
Hypervolemia Treatment
The main aim of the treatment is to reduce the blood volume and to make sure that it does not rise again. For this the cause of hypervolemia should be identified and would have to be treated. General supportive measures will also be required to be done.
- Sodium and water restriction in diet and intravenous fluids (11, 13).
- To reduce the volume of blood, diuretics will have to be given. This also helps to reduce, edema, ascites and pulmonary edema (11, 13).
- Regular monitoring of body weight and urinary output (11, 13).
- In certain cases, isolated ultrafiltration can help to remove the excess fluid and solutes (14).
- Certain drugs to help in vasodilation and to improve pumping of heart, can be used (11, 13).
References:
- https://en.wikipedia.org/wiki/Hypervolemia
- https://www.uptodate.com/contents/general-principles-of-disorders-of-water-balance-hyponatremia-and-hypernatremia-and-sodium-balance-hypovolemia-and-edema
- https://howshealth.com/wp-content/uploads/2014/06/extracellular-and-intracellular-compartments-image.jpg
- http://medicinenet.com/electrolytes/article.htm
- https://emedicine.medscape.com/article/242166-overview
- https://www.sciencedirect.com/topics/medicine-and-dentistry/hypervolemia
- https://www.mja.com.au/journal/2008/189/9/avoiding-common-problems-associated-intravenous-fluid-therapy
- http://www.rcsed.ac.uk/fellows/lvanrensburg/classification/commonfiles/blood_transfusion.htm#Fluidoverload
- http://www.merckmanuals.com/professional/hematology-and-oncology/transfusion-medicine/complications-of-transfusion#sec11-ch146-ch146d-1100
- Page 62 (Fluid imbalances) in: Portable Fluids and Electrolytes (Portable Series). Hagerstwon, MD: Lippincott Williams & Wilkins. 2007
- http://www.hypervolemia.com/
- http://www.pfusion.net/ADAM_IMR/hi1d/ency/article/003077.htm
- https://howshealth.com/hypervolemia/
- https://www.ncbi.nlm.nih.gov/pubmed/495402
Published on February 6th, 2018 by Editorial Team under Diseases and Conditions.
Article was last reviewed on January 12th, 2022.

